
Shelter-in-place, isolation and quarantine can be especially tough on those struggling with mental health concerns. To ease their burden – and without compromising the social-distancing norms intended to curb COVID-19’s spread – the FDA temporarily relaxed some elements of its traditional regulatory review for new digital therapeutics (DTx), specifically those intended to treat psychiatric disorders.
The guidance is one of a number of emergency policies issued by FDA in recent weeks, designed to expand availability of medical devices that it deems low-risk – everything from tools for reviewing digital pathology images to fetal and maternal monitors – during the crisis. The guidance effectively waives the agency’s usual 510(k) premarket notification requirement for these devices, as long as other standards are met.
That came as a welcome surprise to firms like Akili Interactive. The nine-year-old company, which had already been developing a prescription-based attention treatment for children with ADHD, was among the first to take advantage. Akili launched its app on April 22, less than a week after the FDA issued the aforementioned emergency policy.
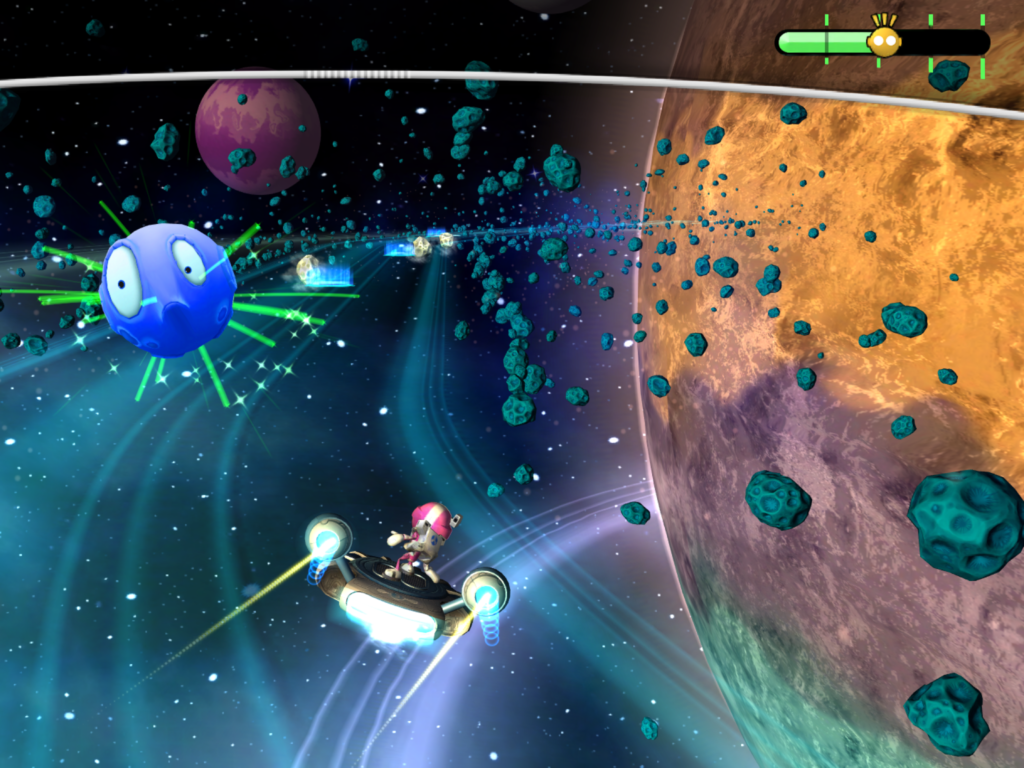
The video game-like app, called Endeavor (AKL-TO1), is being made available, along with a symptom tracker and caretaker support line, to qualifying families with children aged 8 to 12 who have been diagnosed with primarily inattentive or combined-type ADHD. The app, available at no cost for a limited time, is intended to improve attention function.
To find out more about the firm’s remarkably speedy roll-out, and how this temporary access may facilitate uptake of Endeavor among physicians, patients and payers, MM&M caught up with Akili’s VP market access and trade, Jeffrey Abraham. The following interview has been edited for clarity and brevity.
Did you have any indication the FDA was intending to issue this emergency guidance?
No [laughs]. We learned about it when it became public along with the rest of the world.
In essence, then, you had to commercialize the product in a few days, right?
Essentially, it was about a week, give or take, after the guidance came out. It took a couple of days for us to go through [the FDA’s policy], understand what it meant and what we could do. We launched Wednesday morning, so in three to four business days. I heard some of us may have been working over the weekend [laughs]. It put the onus on us. We heard loud and clear [from the guidance]: “If you have something that can help people, get it out there.” And that’s what we did.
What was the internal reaction like, and how did things go over the ensuing hours and days to launch in such a short time?
This is one of the most unique places I’ve ever worked. You have individuals from a lot of different industries and backgrounds. Everybody came together with all our experience and expertise and we got something out very quickly. We [had been] working toward FDA clearance for some time [for] our prescription product, so we were in a really good situation. We had the data to know [this] has a low-risk safety profile. What we really had to do was make sure the product had a good wrap-around experience [and that] people would have an easy time operating and enjoying it.
Prior to COVID-19, Akili was pursuing its own distribution and commercialization platform, foregoing pharma partnerships. Does this new wrinkle help or hinder those efforts?
Getting the product out there now allows us to start improving the [physician and patient] experience from day one. In digital we iterate, we make things better constantly. We’ll start doing that now with what we build out for our patient services, which is a great opportunity.
In terms of commercialization, we get the opportunity to [collect] some learnings about evidence on how people use our product, which helps down the line in terms of partnering with payers, insurers and PBMs. In terms of physicians, we’re already interacting with them now. Part of the guidance is to have some acknowledgement or consultation with an HCP, and so we’re already getting that experience now, even in this COVID-19 situation.
There’s no downside to being able to interact with physicians already and answering their questions and educating them. This is an opportunity for us to start that education early.
(Although Akili has been developing and testing Endeavor as a prescription therapeutic, at this time the FDA is not requiring families to secure a doctor’s order in order to download and use the app, although they are urged to contact a physician about it. -Ed.)
For a DTx company, evidence development, and commercialization based off of that evidence, are key to securing reimbursement. Does this soft launch give you an additional degree of real-world evidence that may help you make your case to payers and physicians?
First and foremost, it was important to get the product out there and help patients. But we absolutely have an opportunity to generate evidence during this time period around how patients are engaging, and an opportunity to help them engage better with our products.
That’s something that’s unique to DTx: Improving the engagement and the user experience actually make your product better as a whole and, in some ways, make it more efficacious. That’s because the more patients who use it, the better it is for them. That’s not necessarily possible in pharma, where you know people fill their pills, and then it stops there. We know when you take your medicine, and we can help with that.
You’ve done a number of randomized controlled clinical trials on the product, but were you nervous at all about releasing this prior to formal FDA clearance?
Our existing evidence base consists of five clinical studies in more than 600 kids with ADHD at this point (including a prospective, randomized controlled study in 348 kids recently published in The Lancet Digital Medicine. -Ed.) Part of what made us so comfortable putting the product out when we did is that we’ve seen the safety and efficacy of the product in a lot of randomized controlled trials and studies. In some of our most recent studies…we’ve started to see more real-world endpoints, scales and metrics more traditionally used in ADHD.
How has COVID-19 affected acceptance of DTx? How are your conversations with payers going?
First and foremost, it’s been, “Does your product help patients?” What’s been super interesting in this time period is, I have seen an altruism come from health insurers, PBMs, health systems and physicians that I personally haven’t experienced before.
Prior to Covid, there was already a spectrum on how [these stakeholders] addressed DTx. There were some who would have already had these conversations, and there are some where the Covid conversation has changed it. But there’s a sense of urgency now that potentially wasn’t quite there before.
That’s what’s shifted during Covid. It really is, “OK, so we have an acute problem now.” Whereas before they may have had an issue that we could have helped them with through our products and services, now it’s a much wider issue and it’s a different issue they’re facing. And DTx has the potential to help.
But we want to be cognizant that…this isn’t an opportunity to just engage and get our product out to other patients, to get access. This isn’t a business opportunity; this is a healthcare crisis. Even amidst our limited access, we still have criteria to make sure it goes to the right patients.
When you say altruism, do you mean a renewed focus on the patient?
It’s not that they don’t focus on the patient first. Being somebody who comes from market access, I genuinely believe people have…their patients’ and members’ best interests at heart. When you see what FDA did with the guidance and what’s happening with telemedicine and digital right now, you’re seeing an expediting of that altruism. People are like, “OK, this is a new situation. As long as it doesn’t hurt people and we have the potential to help people, what’s the best thing we can do?” And that’s not something you hear everyday.
Might this situation change the tide going forward in terms of reimbursement for digital therapeutics?
Similar to what’s happened with telemedicine, you may see some of that happen with DTx and digital medicine, where there’s not just a sense of urgency but the pace to include those products in their benefits and to provide it to their employees and members. You will see that expedited because it’s something that can help [employees and members] today.
How is COVID-19 redefining “value” in healthcare?
Usually value is measured based on your impact to the healthcare system. Well, healthcare today vs. healthcare tomorrow – we don’t know what that’s going to look like. Whereas before, the value of having something in your home that you could access on-demand was important, it’s critical and essential now.
So the definition of value and of showing that value to an insurer, patient and caregiver is changed in this world we’re living in. And we don’t know when it’s going to go back. We’re going to start seeing access [to mental health support] as not a nice-to-have but a must-have, and digital is very uniquely positioned to address that.
The definition of value is, can you help people and can you get to them? The economics of the system are changing so much right now. We don’t know when in-person visits will happen or whether you’ll be able to go back to behavior therapy. And for ADHD, the DEA lifted the in-person requirement for controlled substances. So medication patterns are different, treatment patterns are different.
And the struggles that kids and their parents are facing now are completely different. There’s no sports, there’s no school. You’re doing everything at home, including remote learning. So what’s the definition of value in that context? The intangibles of health economics and outcomes research (HEOR) studies will become a lot more tangible: providing a sense of comfort and a positive experience that comes from healthcare services like a way to measure symptoms and behaviors and a patient support line. All those things will become essential and will redefine value.
The relaxing of the FDA’s 510(k) requirement is only temporary until the end of the pandemic. If and when the agency rescinds its guidance, what do you expect to happen?
That’s a good question. We were actively pursuing FDA clearance for our product. Our intent is not to take it away from patients. But we’ll see what the future brings; this is uncharted territory for everybody. We will work with the FDA no matter the outcome.
This story has been updated to clarify that Endeavor is not a cognitive behavioral therapy app.







