State-accredited CME providers continue to decrease, with 68 dropping out as of last year, but so far the trend has not posed a threat to physician education, one official says.
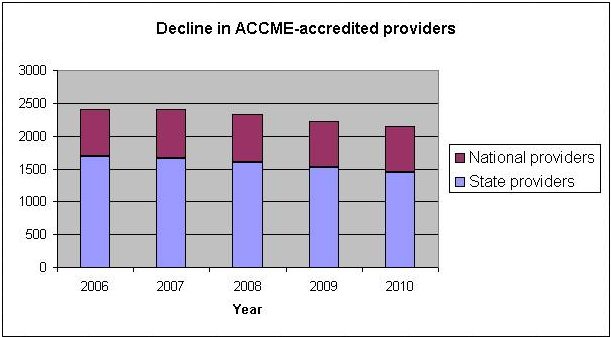
Between 2003 and 2010, the number of providers accredited by state medical societies—so-called intrastate providers—fell by 18.7% to 1,450, according to data from the American Medical Association (AMA) and the Accreditation Council for CME (ACCME). These providers, mostly community hospitals, were responsible for roughly a third of all activities certified for AMA PRA Category 1 Credit last year.
The other two-thirds of activities are presented by ACCME-accredited national providers, of which there are 694. But the activities presented by the small hospitals are critical, notes the AMA, because they address local educational and practice needs that are specific to the patient populations where the physician practices.
Unabated, this trend could “impede the delivery of cost-effective, quality, accessible certified CME” dealing with local health issues, noted an internal report by AMA’s Council on Medical Education (CME Rep. 9-A-11).
A 2010 AMA report had explored the reasons behind the drop-out rate for intrastate providers. One is increased annual accreditation fees.
This year the fees rose from $80 to $250. Two more increases are scheduled, lifting the cost to $450 in 2012 and $550 in 2013. (The ACCME had delayed the increase and is implementing it incrementally, in response to the AMA.) AMA has asked ACCME to reconsider the scheduled fee hikes.
“We agree with the AMA that fees should not be onerous, should not be a burden and should be valid and justified,” said Dr. Murray Kopelow, ACCME chief executive. The ACCME currently plans to implement the increases as scheduled.
The decision was made in 2008 by the ACCME board of directors after recognizing a third of the council’s revenue was being spent on the state system while about 95% of its revenue was coming from the nationally accredited providers. “The board said we should redistribute the expense burden more equitably,” said Kopelow, adding that only 11 providers in the country have yet to pay this year’s higher fee.
Another reason behind the high withdrawal rates of state providers, according to AMA, is ACCME’s updated compliance criteria requiring providers to link activities to practice gaps and evaluate for change in learners’ competence, performance or patient outcomes. ACCME raised that bar in 2006.
In the five years since, 14% of state providers (234) have left the system, compared to 5% (35) of national providers. “But there is a national consensus that this is the CME we want,” said Kopelow. In addition, “all member organizations [including the AMA] approved or had an opportunity to veto those criteria if they wanted.”
Added Kopelow, “The concerns of the AMA of a loss of access, or inappropriate fees or the negative impact of regulations on continuing education—those are very important and very relevant.”
But, he said, “The scope of the enterprise and the amount of participation seems to be the same,” at least at the national level, because some providers switch to joint sponsorship—partnering with another organization that has accreditation—and the CME gets “redistributed.”
Data partially support the redistribution theory. Between 2008 and 2010, national- and state-level providers—combined—drew more MDs to CME courses. But activities were down 15% and hours were down 13% during that period. (Kopelow said part of the decrease is due to the new PARS reporting system, which enabled the ACCME to review information at the activity level and better ensure that providers submitted data in accordance with ACCME definitions of the number of activities and hours.)
Nevertheless, “When the same amount of continuing education can be delivered through one accreditation, that’s highly efficient,” Kopelow said.
At its House of Delegates meeting in June, the AMA agreed to continue working with the ACCME to relieve the state providers and to take up the cost issue at its 2012 annual meeting.